Introduction
Physiotherapy in Beamsville for Pediatric Issues
Welcome to Beamsville Physiotherapy’s resource on Jumper's Knee in Children and Adolescents.
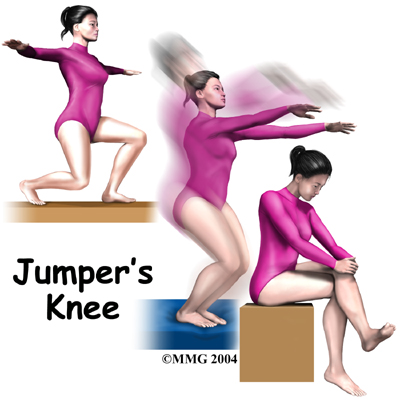 When a child or adolescent complains of pain and tenderness near the bottom of the kneecap, the problem might be from jumper's knee. Kids in sports that require a lot of kicking, jumping, or running are affected most. Repeating these actions over and over can lead to pain in the tendon that stretches over the front of the kneecap (the patellar tendon.)
When a child or adolescent complains of pain and tenderness near the bottom of the kneecap, the problem might be from jumper's knee. Kids in sports that require a lot of kicking, jumping, or running are affected most. Repeating these actions over and over can lead to pain in the tendon that stretches over the front of the kneecap (the patellar tendon.)
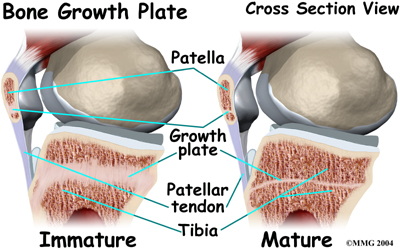
Sometimes the bone growth center at the bottom tip of the kneecap is affected instead of the patellar tendon itself. This condition is known as Sinding-Larsen-Johansson disorder. It is mostly likely to occur during growth spurts. Disruption within the developing bone in the bottom tip of the kneecap also produces pain and tenderness in the front of the knee.
Fortunately, this condition is not serious. It is usually only temporary and will improve with age.
This guide will help you understand:
- what part of the knee is involved
- what causes the condition
- what the condition feels like
- how health care professionals identify the problem
- what treatment options are available
- what Beamsville Physiotherapy’s approach to rehabilitation is
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Pediatrics|limit:15|heading:Hear from some of our *Pediatrics* patients#
Anatomy
What part of the knee is involved?
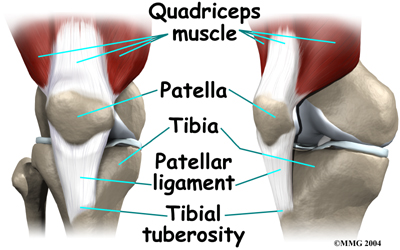 Jumper's knee affects the patellar tendon. The patellar tendon connects the large and powerful quadriceps muscle in the front of the thigh to the tibia (shinbone). The patellar tendon wraps over the front of the patella (kneecap). The upper end of the patellar tendon connects to the bottom tip of the patella. This area is called the inferior pole of the patella. The lower end of the patellar tendon connects to a small bump of bone on the front surface of the tibia. This bump is called the tibial tuberosity.
Jumper's knee affects the patellar tendon. The patellar tendon connects the large and powerful quadriceps muscle in the front of the thigh to the tibia (shinbone). The patellar tendon wraps over the front of the patella (kneecap). The upper end of the patellar tendon connects to the bottom tip of the patella. This area is called the inferior pole of the patella. The lower end of the patellar tendon connects to a small bump of bone on the front surface of the tibia. This bump is called the tibial tuberosity.
Causes
How does this problem develop?
Jumper's knee is usually caused by overuse of the patellar tendon. Kids who play sports with a lot of squatting and jumping are most at risk. In order to squat and to land softly from a jump, the quadriceps muscle must work extra hard to slow the body down and protect the knee. It does this by lengthening as it works, which is called an eccentric contraction. This muscle action places very high tension on the patellar tendon. When squatting and jumping are performed over and over, the repetitive stress on the tendon causes injury to the individual fibers of the tendon. The tendon becomes inflamed and painful. This is the condition called jumper's knee.
 In addition to overuse of the tendon causing the patellar tendon pain, abnormal alignment of the lower limbs can play a major part in the development of jumper’s knee. Kids who are knock-kneed or flat-footed seem to be more prone to the condition. These altered postures cause a sharper angle between the quadriceps muscle and the patellar tendon. This angle is called the Q-angle. Having a large Q-angle puts more tension on the patellar tendon and the risk of developing jumper's knee is thus higher.
In addition to overuse of the tendon causing the patellar tendon pain, abnormal alignment of the lower limbs can play a major part in the development of jumper’s knee. Kids who are knock-kneed or flat-footed seem to be more prone to the condition. These altered postures cause a sharper angle between the quadriceps muscle and the patellar tendon. This angle is called the Q-angle. Having a large Q-angle puts more tension on the patellar tendon and the risk of developing jumper's knee is thus higher.
A large Q-angle also places abnormal tension on the bone growth plate of the inferior pole of the patella, also increasing the risk for Sinding-Larsen-Johansson disorder. A high-riding patella, called patella alta, is also thought to contribute to development of jumper's knee in children and adolescents.
Pain around the patellar tendon pain can start simply from a growth spurt in an active child whose bones are not done growing. Increased tension in the tendon starts during the growth spurt. The patellar tendon is unable to keep up with the growth of the lower leg. As a result, the tendon is too short. This causes the tendon to pull on the bottom tip of the kneecap. Heavy or repetitive sports activity during this time stresses this area even more. Eventually the increased tension disrupts normal growth of the bottom tip of the patella. Again, this is known as Sinding-Larsen-Johansson disorder.
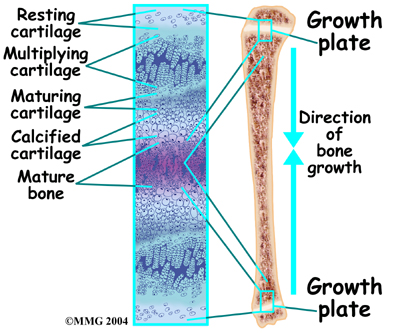 Sinding-Larsen-Johansson disorder is part of a category of bone development disorders known as the osteochondroses. (Osteo means bone, and chondro means cartilage.) In normal development, specialized areas called growth plates change over time from cartilage to bone. The growth plates expand and unite. This is how bones grow in length and width. Bone growth centers are located throughout the body.
Sinding-Larsen-Johansson disorder is part of a category of bone development disorders known as the osteochondroses. (Osteo means bone, and chondro means cartilage.) In normal development, specialized areas called growth plates change over time from cartilage to bone. The growth plates expand and unite. This is how bones grow in length and width. Bone growth centers are located throughout the body.
Children with bone development disorders in one part of their body are likely to develop similar problems elsewhere. For example, children who have Sinding-Larsen-Johansson disorder also have a small chance of bone growth problems where the lower end of the patellar tendon attaches to the tibial tuberosity. This is known as Osgood Schlatter’s disease.
Symptoms
What does this problem feel like?
Jumper's knee commonly produces pain and tenderness directly over the patellar tendon, just below the kneecap. Sometimes there is a small amount of swelling. Kneeling on the sore knee usually hurts. Activities where the quadriceps muscle works eccentrically, such as squatting, jumping, and going down stairs, are often painful.
Kids with Sinding-Larsen-Johansson disorder may feel similar symptoms right along the bottom of the kneecap, where the patella meets the patellar tendon. Sometimes they feel tightness in this area, especially when they try to fully bend the knee.
Diagnosis
How do health care professionals identify the problem?
The history and physical examination are often enough to suspect a diagnosis of jumper's knee. Your physiotherapist at Beamsville Physiotherapy will ask many questions and will want information about your child's age and activity level. They will also ask about where precisely the pain is, when the pain began, what your child was doing when the pain started, and what movements aggravate or ease the pain. Jumper’s knee generally begins insidiously, but on occasion it can be instigated by a trauma to the knee such as a fall or hard knock to the knee.
Next your physiotherapist will do a physical examination of the knee and entire lower extremities. They will palpate, or touch, around the knee and particularly along the patella and patellar tendon to determine the exact location of pain. Your physiotherapist will look for factors such as bony alignment (Q-angle,) muscle flexibility, mobility of the patella, and joint laxity that may be contributing to your child’s knee pain. They may want to look at how your child stands, their foot position, or watch them walk, squat, or jump. Your physiotherapist will also check the strength and lengths of the muscles surrounding and affecting the knee joint such as the quadriceps, hamstrings, calves, hip flexors and buttocks muscles. All of these muscles, if weak or tight, can contribute to the forces applied to the knee joint and contribute to the development of jumper’s knee. They may also assess your child’s core stability (specific lumbar and abdominal muscles) as poor functioning of the core can also contribute to the development of knee problems.
Lastly, resistance while your child straightens their knee will be checked to see if it elicits pain. This action generally reproduces the pain associated with jumper’s knee because it puts tension on the patellar tendon.
If Sinding-Larsen-Johansson disorder is suspected, it is wise to have an X-ray. The X-ray is taken from the side of the knee. This view may show small fragments of bone where tension in the patellar tendon has disrupted the growth plate in the bottom tip of the patella. The X-ray may also show calcification or roughness around the bottom of the patella.
If a trauma to the knee instigated the pain then an X-ray is also required to rule out a patellar fracture.
An ultrasound may also be suggested as a way to directly view any damage to the patellar tendon itself, but it is not frequently needed to confirm the diagnosis.
Occasionally, a magnetic resonance imaging (MRI) scan will be ordered in addition to an X-ray as it may show more detail. The MRI can give a better view of any calcification in the patellar tendon where it attaches on the bottom tip of the kneecap. The MRI can also detect swelling, which is not seen well on X-ray. It can also show if injury or inflammation is present within the patellar tendon itself.
Beamsville Physiotherapy provides services for physiotherapy in Beamsville.
Treatment
What treatment options are available?
Nonsurgical Rehabilitation and Treatment
In the case of Sinding-Larsen-Johansson disorder, the disease is often self-limiting, which means that with a certain passing of time, the pain will entirely go away. This time frame coincides with the bone growth plates that form the inferior pole of the patella growing together to form one solid bone. This generally takes one to two years. Once the bones have grown together, the pain and symptoms usually go away completely. Physiotherapy treatment at Beamsville Physiotherapy during this time, while the bones are still growing together, can be very useful to manage the injury by decreasing pain and inflammation, as well as to monitor the appropriate level of physical activity that your child partakes in. For true jumper’s knee, where the patellar tendon itself if affected and not the growth plate, physiotherapy is also very useful for the same reasons.
In some cases of jumper's knee, your child may need to stop sports activities for a short period. This allows the pain and inflammation to settle. Usually patients don't need to avoid sports for a long time. ‘Relative rest’ may be suggested rather than a complete cessation of physical activity. ‘Relative rest’ is a term used to describe a process of rest-to-recovery based on the severity of symptoms. If your child is experiencing pain while doing nothing (resting) it means the injury is more severe and your physiotherapist will advise a period of strict cessation of activity. If, however, your child’s pain is not severe and only occurs intermittently with certain activities or after activity, then your child may be able to continue to partake in a moderate amount of activity (relative rest) while being treated for jumper’s knee. Your physiotherapist will provide advice on the appropriate activity level that your child can safely partake in while dealing with their jumper’s knee.
The initial treatment for jumper’s knee at Beamsville Physiotherapy will aim to decrease the inflammation and pain in the knee. Simply icing the knee can often assist with the inflammation and relieve a great deal of the pain. In cases of chronic pain (lasting longer than 3 months), heat may be more useful in decreasing pain. Your physiotherapist may also use electrical modalities such as ultrasound or interferential current to decrease the pain and inflammation. Massage, particularly for the quadriceps muscle, may also be helpful.
Medication to ease the pain or inflammation can often be very beneficial in the overall treatment of jumper’s knee. Your physiotherapist may suggest you see your doctor to discuss the use of anti-inflammatories or pain-relieving medications in conjunction with your physiotherapy treatment. Your physiotherapist may even liaise directly with your doctor to obtain their advice on the use of medication in your individual case, and suggest you see them if they feel it would be beneficial.
Cortisone injections performed by a doctor are commonly used to control pain and inflammation in other types of injuries involving the patellar tendon, however, a cortisone injection is usually not appropriate for this condition. Cortisone injections haven't shown consistently good results for jumper's knee and there is also a high risk that the cortisone will cause the patellar tendon to rupture.
Once the initial pain and inflammation has calmed down, your physiotherapist will focus on improving the flexibility, strength, and alignment around the knee joint and entire lower extremity. Static stretches for the muscles and tissues around the knee (particularly the quadriceps and iliotibial band on the outside of the knee) will be prescribed by your physiotherapist early on in your treatment to improve flexibility.
Again, any tightness in the muscles or tissues around the knee can increase the pull on the patellar tendon or affect alignment during walking, running or jumping so it is important to address this immediately. Dynamic stretching (rapid motions that stretch the tissues quickly, similar to that of an eccentric contraction,) will also be taught and will be incorporated into your child’s rehabilitation exercise routine as part of their warm-up when doing more physical activity. Dynamic stretches more effectively prepare the tissues for rapid and repetitive activity than static stretches, which focus more on gaining overall flexibility.
Strength imbalances will also affect the alignment of the knee and can cause muscles to tighten which puts more pressure on the knee and can contribute to the cause of jumper’s knee. Your physiotherapist will determine which muscles in your child’s individual case require the most strengthening. Strength in both the knee and the hip (which controls the knee position) are very important. When bending the knee, as stated above, the patellar tendon is placed under load while it is stretching (eccentric load.) This load can be tremendous especially when jumping and landing. In order to prepare the healing tendon to take this load once your child returns to activity your physiotherapist will prescribe ‘eccentric’ muscle strengthening. Bending the knee quickly into a squatting position and then stopping rapidly (drop squats) encourages the patellar tendon (and entire knee joint) to adapt to the force that will eventually be needed to return to physical activity. When appropriate, weights can be added to simulate the increased body weight that the knee endures during running and jumping.
Your physiotherapist may ask your child to do this exercise on a board slanting downwards (approximately 25 degrees) which has been shown to also increase the force through the tendon. In addition, an electrical muscle stimulator may be used on the quadriceps muscle during the activity which encourages improved recruitment of the muscle, particularly the medial quadriceps portion which has a considerable effect on the position of the patella and pull on the patellar tendon. All exercises should be completed with minimal or no pain and advancing the exercises should be done at the discretion of your physiotherapist as not to flare up the healing tendon. Once these exercise are mastered, your physiotherapist may add even more advanced exercises such as jumping and landing from a height or on different surfaces.
As part of your treatment your physiotherapist may choose to use a hands-on technique to mobilize your kneecap and improve its flexibility. In cases where the patella does not move well, improved movement can change the overall pull on the patellar tendon and therefore assist in decreasing overall pain.
Bracing or taping the knee or kneecap may also help your child do exercises and activities with less pain. Your physiotherapist can educate you on which brace would be most appropriate for your child but an initial trial of taping is an easy and cost-effective way to determine if a brace will in fact decrease your child’s pain before actually investing in one. Your physiotherapist may even teach your child how to tape their own knee or show you how to do it for them. Taping over a longer time frame will cause irritation to the skin and can be cumbersome, therefore if the taping helps, a brace, which performs a similar function, may be suggested. Braces used for jumper’s knee are made of soft fabric, such as cloth or neoprene. There are different types of braces that may help. The braces work by one of two mechanisms. They either work to encourage proper alignment of the patella as it glides down the knee, and therefore decreases the abnormal pull on the patellar tendon, or the brace presses into the patellar tendon itself and distributes the force of the load through a greater region of the patellar tendon. Patients commonly report less pain and improved function with both taping and bracing.
As mentioned above, proper alignment of your child’s entire lower extremity is paramount to decreasing the overall stress that is placed on the patellar tendon. In addition to strengthening, stretching, hands-on treatment, and taping, foot orthotics may be useful to assist with alignment. Foot orthotics can correct a flat foot position, which in turn then encourages proper alignment up the lower extremity chain. Your physiotherapist can advise you on whether orthotics would be useful for your child, and also on where to purchase them.
A critical part of our treatment for jumpers knee at Beamsville Physiotherapy includes specific education on returning to full physical activity. Bending and straightening the knee occurs often in everyday activities such as walking or stair climbing so a patellar tendon that is recovering from injury can easily be aggravated. Returning your child back to normal physical activity at a graduated pace is crucial to avoid repetitive pain or a chronic injury. Your physiotherapist will advise you on the acceptable level of activity at each stage of your child’s rehabilitation process and assist your child in returning to his or her activities as quickly and as safely as possible.
With a well-planned rehabilitation program and adherence to suggested levels of rest and activity modification, most children and adolescents dealing with jumper’s knee or Sinding-Larsen-Johansson disorder eventually recover fully without recurring symptoms. By following the rehabilitation plan, most children are also able to partake in a level of activity that suits them while recovering.
Beamsville Physiotherapy provides services for physiotherapy in Beamsville.
Surgery
Surgery is rarely needed for jumper's knee. Surgery may be considered if the problem involves only the tendon (not the growth plate) and if symptoms have not gone away with other forms of treatment. In these cases, the surgeon may do an operation to strip away (debride) inflamed and damaged tissue on the surface of the patellar tendon.
In this procedure, a small incision is made down the front of the knee, below the patella.
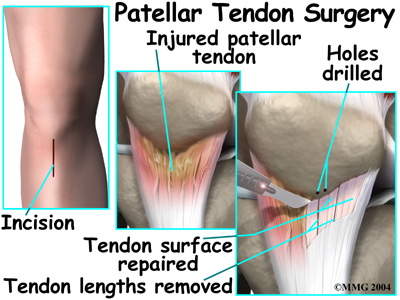 The skin is opened to expose the patellar tendon. Next, the surgeon carefully peels damaged tissue off the surface of the tendon. Three to five thin lengths of the tendon are removed. In some cases, small drill holes are made in the bottom tip of the patella. This drilling causes a small amount of bleeding, which signals the body to begin to heal the area. The surgeon also removes any damaged tissue nearby the area before completing the operation by stitching up the skin and wrapping the area with a bandage.
The skin is opened to expose the patellar tendon. Next, the surgeon carefully peels damaged tissue off the surface of the tendon. Three to five thin lengths of the tendon are removed. In some cases, small drill holes are made in the bottom tip of the patella. This drilling causes a small amount of bleeding, which signals the body to begin to heal the area. The surgeon also removes any damaged tissue nearby the area before completing the operation by stitching up the skin and wrapping the area with a bandage.
Surgery is not generally used when symptoms are caused by Sinding-Larsen-Johansson disorder, unless bone growth is complete and symptoms have not gone away with nonsurgical treatment. Even then, surgery for Sinding-Larsen-Johansson disorder is unusual.
After Surgery
The surgeon may recommend wearing a hinged knee brace for a few weeks after surgery. The brace lets the knee bend, but it doesn't let the quadriceps muscle fully straighten the knee. This decreases the amount of force put through the healing tendon. Crutches may be needed for a few days after the operation, until the patient can bear weight without pain or problems, and walk without a limp.
Patients will follow up with their surgeon 10 to 14 days after surgery. Stitches will be taken out at this time, and patients are encouraged to begin actively bending and straightening the knee. Post-surgical rehabilitation at Beamsville Physiotherapy can begin at this time.
Post Surgical Rehabilitation
Post-surgical rehabilitation at Beamsville Physiotherapy will initially focus on minimizing the pain and swelling from the surgery. Similar to non-surgical rehabilitation, your physiotherapist may use modalities such as ice, ultrasound, or interferential current to accomplish this. They may also use gentle massage around the muscles of your child’s surgical knee. If your child is still using crutches when we initially see them, your physiotherapist will ensure your child knows how to use them properly on level ground as well as stairs, and they will advise your child when it is safe to go without using the crutches at all.
One of the first exercises your physiotherapist will prescribe will be some gentle range of motion exercises for your knee to gradually regain full movement. This should be done within a pain free range of motion, however, movement will be encouraged even if it causes a slight bit of discomfort as the movement itself can greatly assist with dispersing any inflammation as well as improving the overall level of pain. A stationary bicycle can be very useful in the initial stages of gaining range of motion in the knee, so if able, you will be encouraged to use one. Even if you are unable to fully rotate the pedals, the back and forth motion on the bike is an excellent method of slowly encouraging the knee to regain its full range of motion.
Once the pain and swelling is under control your child’s rehabilitation will follow a similar pattern to that described above under non-surgical rehabilitation. Your physiotherapist will prescribe a series of exercises that address the strength, endurance, and flexibility of the muscles of the knee and hip joints. They will also address the overall alignment of the entire lower limb during both the rehabilitation exercises as well during everyday activities and sporting endeavors. Eccentric exercises are an important part of post-surgical rehabilitation and will be introduced as soon as your physiotherapist feels it is appropriate.
Daily activities will be resumed fairly quickly but vigorous activities and exercise should be avoided for at least six weeks after surgery to give adequate rest to the healing tendon. High-level athletes, unfortunately, may be restricted in their sporting activities for up to six months to allow the tendon to heal and to ensure there is not a recurrence of the injury.
Recovery from surgery for jumper’s knee in adolescents or children generally progresses very well with rehabilitation at Beamsville Physiotherapy. If however, your child’s pain lasts longer than it should or their rehabilitation is not progressing as quickly as your physiotherapist feels it should be, they will ask you to follow up again with your child’s surgeon to ensure there are no complicating factors impeding the recovery.
Beamsville Physiotherapy provides services for physiotherapy in Beamsville.
Portions of this document copyright MMG, LLC.
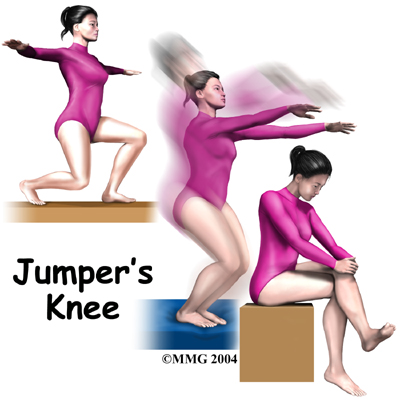 When a child or adolescent complains of pain and tenderness near the bottom of the kneecap, the problem might be from jumper's knee. Kids in sports that require a lot of kicking, jumping, or running are affected most. Repeating these actions over and over can lead to pain in the tendon that stretches over the front of the kneecap (the patellar tendon.)
When a child or adolescent complains of pain and tenderness near the bottom of the kneecap, the problem might be from jumper's knee. Kids in sports that require a lot of kicking, jumping, or running are affected most. Repeating these actions over and over can lead to pain in the tendon that stretches over the front of the kneecap (the patellar tendon.)








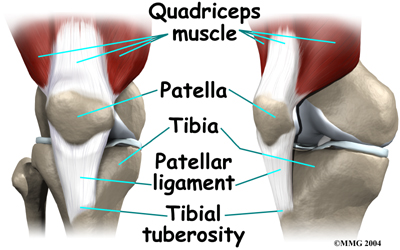 Jumper's knee affects the patellar tendon. The patellar tendon connects the large and powerful quadriceps muscle in the front of the thigh to the tibia (shinbone). The patellar tendon wraps over the front of the patella (kneecap). The upper end of the patellar tendon connects to the bottom tip of the patella. This area is called the inferior pole of the patella. The lower end of the patellar tendon connects to a small bump of bone on the front surface of the tibia. This bump is called the tibial tuberosity.
Jumper's knee affects the patellar tendon. The patellar tendon connects the large and powerful quadriceps muscle in the front of the thigh to the tibia (shinbone). The patellar tendon wraps over the front of the patella (kneecap). The upper end of the patellar tendon connects to the bottom tip of the patella. This area is called the inferior pole of the patella. The lower end of the patellar tendon connects to a small bump of bone on the front surface of the tibia. This bump is called the tibial tuberosity. In addition to overuse of the tendon causing the patellar tendon pain, abnormal alignment of the lower limbs can play a major part in the development of jumper’s knee. Kids who are knock-kneed or flat-footed seem to be more prone to the condition. These altered postures cause a sharper angle between the quadriceps muscle and the patellar tendon. This angle is called the Q-angle. Having a large Q-angle puts more tension on the patellar tendon and the risk of developing jumper's knee is thus higher.
In addition to overuse of the tendon causing the patellar tendon pain, abnormal alignment of the lower limbs can play a major part in the development of jumper’s knee. Kids who are knock-kneed or flat-footed seem to be more prone to the condition. These altered postures cause a sharper angle between the quadriceps muscle and the patellar tendon. This angle is called the Q-angle. Having a large Q-angle puts more tension on the patellar tendon and the risk of developing jumper's knee is thus higher.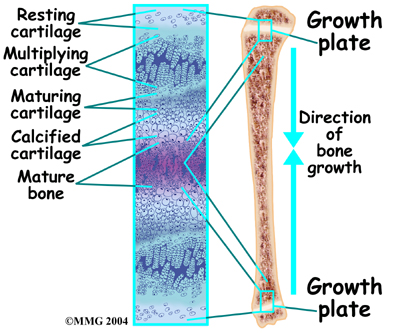 Sinding-Larsen-Johansson disorder is part of a category of bone development disorders known as the osteochondroses. (Osteo means bone, and chondro means cartilage.) In normal development, specialized areas called growth plates change over time from cartilage to bone. The growth plates expand and unite. This is how bones grow in length and width. Bone growth centers are located throughout the body.
Sinding-Larsen-Johansson disorder is part of a category of bone development disorders known as the osteochondroses. (Osteo means bone, and chondro means cartilage.) In normal development, specialized areas called growth plates change over time from cartilage to bone. The growth plates expand and unite. This is how bones grow in length and width. Bone growth centers are located throughout the body.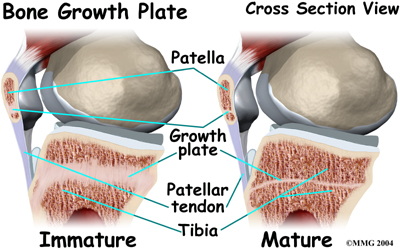
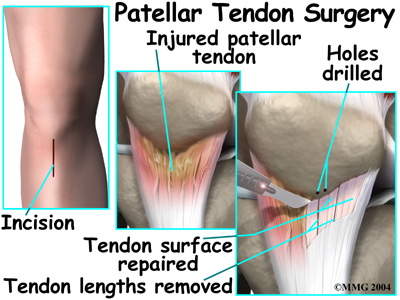 The skin is opened to expose the patellar tendon. Next, the surgeon carefully peels damaged tissue off the surface of the tendon. Three to five thin lengths of the tendon are removed. In some cases, small drill holes are made in the bottom tip of the patella. This drilling causes a small amount of bleeding, which signals the body to begin to heal the area. The surgeon also removes any damaged tissue nearby the area before completing the operation by stitching up the skin and wrapping the area with a bandage.
The skin is opened to expose the patellar tendon. Next, the surgeon carefully peels damaged tissue off the surface of the tendon. Three to five thin lengths of the tendon are removed. In some cases, small drill holes are made in the bottom tip of the patella. This drilling causes a small amount of bleeding, which signals the body to begin to heal the area. The surgeon also removes any damaged tissue nearby the area before completing the operation by stitching up the skin and wrapping the area with a bandage.