Introduction
Physiotherapy in Beamsville for Hip Issues
Welcome to Beamsville Physiotherapy's resource about femoroacetabular impingement.
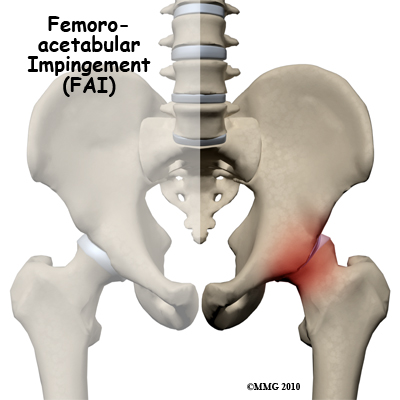
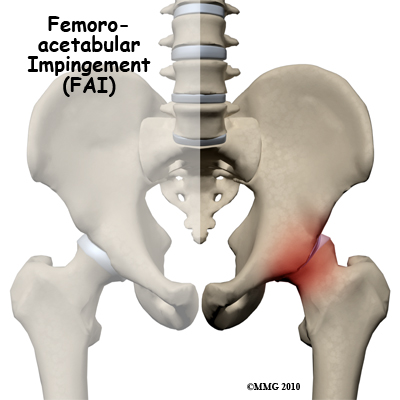 Femoroacetabular impingement (FAI) occurs in the hip joint. Impingement refers to some portion of the soft tissue around the hip socket getting pinched or compressed. Femoroacetabular tells us the impingement is occurring where the femur (thigh bone) meets the acetabulum (hip socket). There are two different types of impingement. They differ slightly depending on what gets pinched and where the impingement occurs.
Femoroacetabular impingement (FAI) occurs in the hip joint. Impingement refers to some portion of the soft tissue around the hip socket getting pinched or compressed. Femoroacetabular tells us the impingement is occurring where the femur (thigh bone) meets the acetabulum (hip socket). There are two different types of impingement. They differ slightly depending on what gets pinched and where the impingement occurs.
This guide will help you understand:
- what parts of the hip are involved
- how the problem develops
how health care professionals diagnose the condition
- what treatment options are available
- what Beamsville Physiotherapy’s approach to rehabilitation is
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Hip Pain|limit:15|heading:Hear from some of our patients who we treated for *Hip Pain*#
Anatomy
What part of the body is affected?
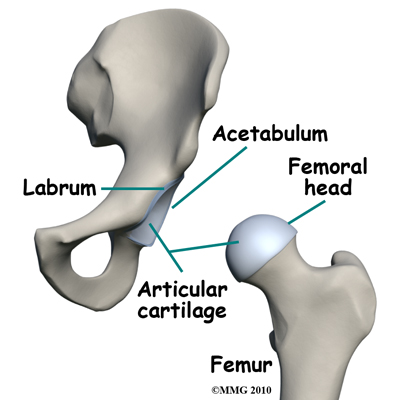
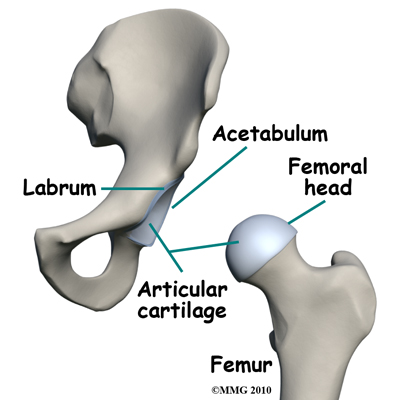 Femoroacetabular refers to the place in the hip where the round head of the femur (thigh bone) comes in contact with the acetabulum or hip socket. Two types of impingement are known to cause pinching of the soft tissues in this area: The first is called cam-type impingement. This occurs when the round head of the femur isn't as round as it should be. It's more of a pistol grip shape.
Femoroacetabular refers to the place in the hip where the round head of the femur (thigh bone) comes in contact with the acetabulum or hip socket. Two types of impingement are known to cause pinching of the soft tissues in this area: The first is called cam-type impingement. This occurs when the round head of the femur isn't as round as it should be. It's more of a pistol grip shape.
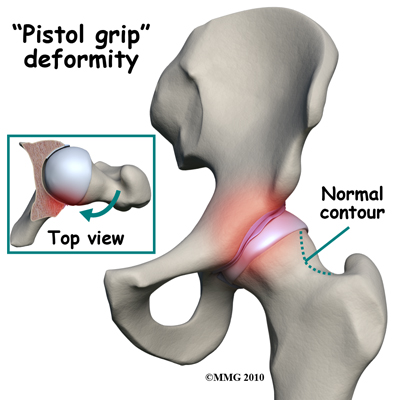
It's even referred to as a pistol grip deformity. The femoral head isn't round enough on one side (and it's too round on the other side) to move properly inside the socket.
The result is a shearing force on the labrum and the articular cartilage, which is located next to the labrum. The labrum is a dense ring of fibrocartilage firmly attached around the acetabulum (socket). It provides depth and stability to the hip socket. The articular cartilage is the protective covering over the hip joint surface.
Sometimes cam-type impingement occurs as a result of some other hip problem (e.g. Legg-Calve-Perthes disease, slipped capital femoral epiphysis,) but most of the time, it occurs by itself and is the main problem. Men are affected by cam-type impingement more often than women.
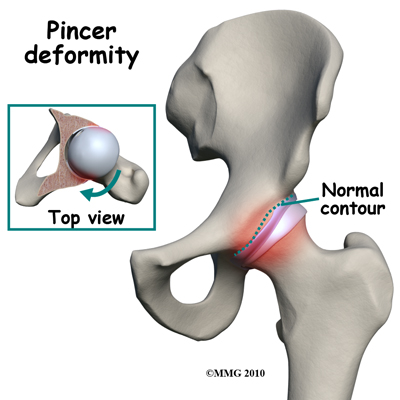
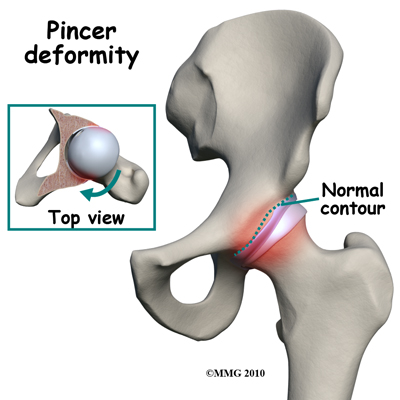
The second type of impingement is called pincer-type impingement (more common in women). In this type, the socket covers too much of the femoral head. As the hip moves, the labrum comes in contact with the femoral neck just below the femoral head.
Pincer-type impingement is usually caused by some other problem. It could be as a result of 1) hip dysplasia, 2) a complication after osteotomy surgery (cutting away bone) to correct hip dysplasia, or 3) an abnormal position of the acetabulum called retroversion. Hip dysplasia is a deformity of the hip (either of the femoral head or the acetabulum, or both) that can lead to hip dislocation.
Causes
What causes this problem?
The cause of the problem has been under considerable debate for a long time. Now with better imaging studies, we know that some subtle changes in the shape of the femoral head may be the cause of FAI. Other anatomical changes in the angle of the hip may also contribute to this problem.
The basic problem is that the head of the femur butts up against the cartilage rim around the acetabulum and pinches it. An alternate type of femoral acetabular impingement causes abnormal jamming of the head-neck junction.
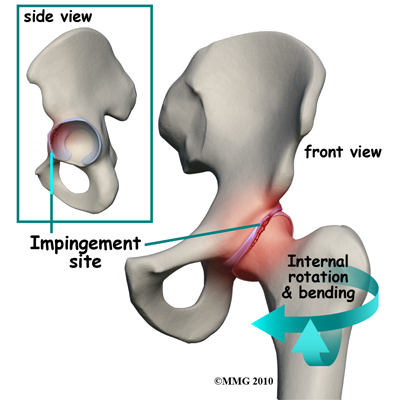 Normally, the femoral head moves smoothly inside the hip socket. The socket is just the right size to hold the head in place. If the acetabulum is too shallow or too small, the hip can dislocate. In the case of FAI, the socket may be too deep.
The rim of the cartilage hangs too far over the head. When the femur flexes (bends) and internally rotates, the cartilage gets pinched. Over time, this pinching or impingement of the labrum can cause fraying and tearing of the edges and/or osteoarthritic changes at the impingement site.
At the same time, with changes in the shape and structure of the hip, there are changes in normal hip movement. There may be too much hip adduction and internal rotation. Hip adduction refers to movement of the leg toward the body. Muscle weakness of the hip abductor muscles, hip extensors, and hip external rotators add to the problem. Hip abduction is moving the leg away from the body.
With the combined effects of anatomic changes in the hip and the resultant muscle imbalances, repetitive motions can create mini-traumas to the hip joint. The result can be an additional problem: partial or complete labral tears. A complete rupture is referred to as an avulsion which indicates that the labrum is separated from the acetabular cartilage where it normally attaches.
Normally, the femoral head moves smoothly inside the hip socket. The socket is just the right size to hold the head in place. If the acetabulum is too shallow or too small, the hip can dislocate. In the case of FAI, the socket may be too deep.
The rim of the cartilage hangs too far over the head. When the femur flexes (bends) and internally rotates, the cartilage gets pinched. Over time, this pinching or impingement of the labrum can cause fraying and tearing of the edges and/or osteoarthritic changes at the impingement site.
At the same time, with changes in the shape and structure of the hip, there are changes in normal hip movement. There may be too much hip adduction and internal rotation. Hip adduction refers to movement of the leg toward the body. Muscle weakness of the hip abductor muscles, hip extensors, and hip external rotators add to the problem. Hip abduction is moving the leg away from the body.
With the combined effects of anatomic changes in the hip and the resultant muscle imbalances, repetitive motions can create mini-traumas to the hip joint. The result can be an additional problem: partial or complete labral tears. A complete rupture is referred to as an avulsion which indicates that the labrum is separated from the acetabular cartilage where it normally attaches.
Symptoms
What does this condition feel like?
The first noticeable symptom of femoroacetabular impingement is often deep groin pain with activities that stress hip motion. Prolonged walking is especially difficult. Although the condition is often present on both sides, the symptoms are usually only felt on one side. In some cases, the groin pain doesn't start until the person has been sitting and starts to stand up. There is often a slight limp because of pain and limited motion.
Groin pain associated with femoroacetabular impingement can be accompanied by clicking, locking, or catching when chronic impingement has resulted in a labral tear.
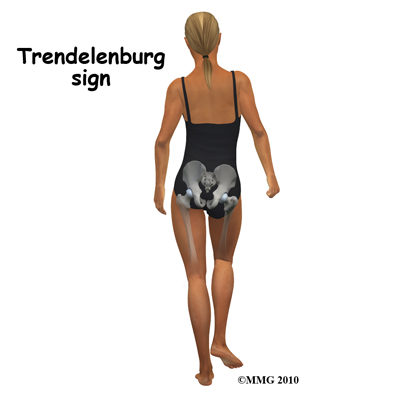
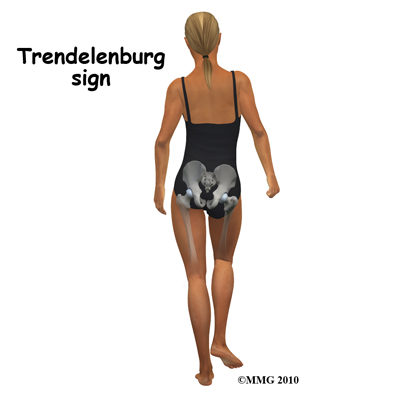
When femoroacetabular impingement and a labral tear are both present, symptoms get worse with long periods of standing, sitting, or walking. Pivoting on the involved leg also reproduces the pain. Some patients have a positive Trendelenburg sign (hip drops down on the right side when standing on the left leg and vice versa).
As is often the case, one problem can lead to others. With femoroacetabular impingement, hip bursitis can develop. The gluteal (buttock) muscles may be extra tender or sore from trying to compensate and correct the problem. The pain can be constant and severe enough to limit all recreational activities and sports participation.
Diagnosis
How do health care professionals diagnose the problem?
Diagnosis begins with a complete history of your injury. Your physiotherapist at Beamsville Physiotherapy will ask questions about where precisely the pain is, when the pain began, if there was a specific injury that occurred or whether the pain gradually developed over time, and what movements aggravate or ease the pain. They will inquire about any previous injuries to the hip, low back, knee or even ankle, which may have contributed to the hip or groin pain you are feeling now. Your therapist will also ask about any swelling, clicking, catching, or weakness in the hip or groin area.
Next they will do a physical examination. Your physiotherapist will first look at your posture and alignment in standing. They may also check to see if you have a leg length discrepancy that is contributing to your injury or dropped arches that can also change your entire lower limb alignment. Next they will palpate all around your low back, pelvis, groin, and also the side and back part of your hip including into your buttocks muscles in order to determine your most tender point. After determining your most sore point they will check the range of movement in your hip by passively moving your hip into many different ranges of motion. Motion in your pelvis and low back may also need to be checked. With FAI often the range of movement of the involved hip is not the same as the normal hip. Depending on the cause of the FAI the range of motion may appear to be restricted or may even appear to be overly mobile, particularly in one direction. In addition the muscles both at the front and back of the hip joint may be tighter than they should be.
The strength of your muscles around your groin and hip as well as your knee and core will be assessed next. Your therapist will ask you to resist certain movements while checking for pain as well as strength deficits. Often with FAI the gluteal muscles are weak on the affected side, which creates a muscular imbalance affecting the biomechanics at the hip. Your therapist may also want to watch you do things such as walk, jog, mini squat on one leg, or hop in order to assess your overall biomechanics.
Other specific tests may be done to provoke your symptoms and test for excess or restricted movement at the hip joint. In one common test done for FAI the patient lies on the table on his or her back. Your physiotherapist then bends your leg up, internally rotates the hip, and presses the knee toward the other leg. This position puts the hip in such a position that impingement occurs and often reproduces the painful symptoms. If you have an inflamed bursa at the front of the hip, this position will also be irritating for it.
Several imaging tests can be done to identify what's going on including X-rays, magnetic resonance images (MRI), and computed tomography (CT) scans. X-rays show the presence of any extra bone build up as well as the position and alignment of the bones and joint. X-rays also show the shape of the femoral head.
Any asymmetries (i.e., where the head is not an even round shape compared to the other side) are also visible on X-rays as well as indications for a retroverted hip, which is, in simple terms, a hip bone that is angled backwards.
MRIs can show any damage to the labrum but not necessarily any changes to the surface of the hip joint. The presence of edema (swelling) under the bone may show up and requires further evaluation to decide if it is from femoroacetabular impingement or some other cause (e.g., cyst, tumor, stress fracture). Using MRI with a dye injected into the joint (called magnetic resonance arthrography or MRA) provides greater detail of the joint surface and may be needed.
CT scans help show the exact shape of the bone and reveal any abnormalities in the bone structure. CT scans might be the most helpful when arthroscopic surgery is planned as they give the surgeon a better idea of what needs to be done to reshape the bone. If the procedure is going to be done with an open incision, then the CT scan isn't necessary, as the surgeon will see everything once the area is opened up.
Treatment
What can be done for this condition?
Once all the test results are available, a course of action is determined. This may be conservative care (nonoperative) with anti-inflammatories and physiotherapy or it may be surgery. Generally patients undergo a trial of conservative care before doing any surgery but in some cases, surgery is recommended right away.
Nonsurgical Rehabilitation
Physiotherapy at Beamsville Physiotherapy can be very helpful for FAI. The goals of conservative management are to relieve pain, improve function by correcting muscle strength imbalances and alignment, and prevent future issues with the hip.
During your first few appointments at Beamsville Physiotherapy your physiotherapist will focus on relieving your pain and inflammation simply to settle the hip down. They may use modalities such as ice, heat, ultrasound, or electrical current. In addition, your physiotherapist may massage your hip or leg to improve circulation and help decrease your pain. Another crucial step to settling your pain down is activity modification. Your therapist will discuss this with you. It is nearly impossible to give the hip a complete rest but avoiding activities such as pivoting on the involved leg when there is a labral tear or irritation, and avoiding long periods of sitting can give the hip a chance to calm down. All sports should also be avoided in these initial stages as should prolonged walking. Sometimes it is necessary to reduce your normal activity in some respect for up to six months in order to let the tissues around the hip joint heal. Your physiotherapist will closely guide you regarding activity modification and will give suggestions for maintaining physical fitness while dealing with this injury.
Based on your individual assessment findings your therapist will design a program of stretches and strengthening exercises specifically for you to help improve the biomechanical function of the hip, the range of motion of the hip, and alter any muscle imbalances that may be present.
Tight muscles around the hip can contribute to pinching between the femoral head and acetabulum in certain positions. Your physiotherapist will give you stretches for both the front and back parts of your hip which includes, in particular, the hip flexors and the external rotators and abductor muscles (deep gluteals) of the hip. They may also ask you to do groin or knee stretches depending on their assessment findings. A program of flexibility for the joint and stretching exercises won’t change any bony abnormalities present but can help lengthen the muscles, correct muscle imbalances, and reduce bony contact and subsequent impingement in the hip. If completing your exercises is difficult, your therapist may suggest you initially go into a hydrotherapy pool where the warmth and hydrostatic properties of the water can assist your discomfort. As soon as you are able, however, your physiotherapist will encourage you to start completing your exercises on land to more closely simulate regular activities of daily living.
Strengthening exercises will focus on correcting any muscle imbalances that have developed as a result of your injury. It is most common that the gluteal muscles, which are the major supporters of the hip as well as rotators, abductors and extensors of the hip, are weak in comparison to other muscles around the hip. This can contribute to the impingement at the hip. Exercises for the gluteals as well as other areas such as the groin, anterior hip, and core area may be prescribed based on your individual assessment findings. Exercise bands, weights or weight machines may be used to add extra resistance and help to build up strength and endurance.
Your therapist will discuss your lower limb alignment, overall posture, and any abnormal movement patterns you may have developed. Sometimes even small changes in your posturing particularly as you walk, such as changing your foot or knee position, can make a significant difference in the pain you feel and how quickly your hip improves. In some cases orthotics to improve arch alignment or a heel lift to correct a leg length discrepancy can make a difference.
When both legs have nearly equal strength, it is possible to gradually resume a full and normal level of all activities (so long as there is no pain during any of those movements or activities).
For the young or active adult, this includes activities of daily living as well as recreational and competitive sports participation. Older adults experiencing labral tears associated with the impingement problem may expect to be able to resume normal daily functions but may still find it necessary to limit prolonged sitting or standing positions.
Your physiotherapist will closely guide your activity levels during your return to activity in order to ensure you don’t overdo any aspect and to ensure that you avoid re-injuring the hip.
You physiotherapist at Beamsville Physiotherapy will liaise with your doctor regarding your progress with rehabilitation. While undergoing physiotherapy treatment some patients may also benefit from intra-articular injection from a doctor. This injection combines a numbing agent with an anti-inflammatory (steroid) medication in order to calm the hip down and allow you to strengthen and stretch the hip.
If conservative care does not relieve your problem, surgery may be required. It should be noted, however, that anyone needing surgery will also benefit from physiotherapy prior to the surgical procedure in order to address any muscle imbalances and abnormal movement patterns that may have contributed to the FAI.
Beamsville Physiotherapy provides services for physiotherapy in Beamsville.
Surgery
Surgery is advised when there is persistent pain despite a good effort at conservative care and when there are obvious structural abnormalities of the hip. Early diagnosis and surgical correction may be able to restore normal hip motion. Delaying surgery is possible for some patients but the long-term effects of putting surgery off have not been determined.
Once it has been decided that surgery is the way to go, the surgeon has three choices: 1) full open incision and correction of the problem, 2) arthroscopic surgery, and 3) osteotomy (cutting the bone to reshape the socket.)
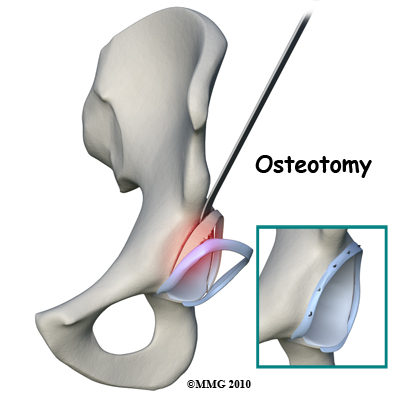 With the fully open surgical procedure, the head of the femur is dislocated from the socket to make the changes and corrections and reshape it. With arthroscopic surgery, hip dislocation is not required. Osteotomy is done for pincer-type impingement.
Whenever possible, the surgeon tries to save the hip. When there is extensive damage to the cartilage, hip resurfacing or total joint replacement may be needed. There are many factors to consider when making the decision whether or not to do a hip replacement. These factors include the patient's age, findings on imaging studies, type and severity of deformity, as well as the presence of arthritic changes.
With the fully open surgical procedure, the head of the femur is dislocated from the socket to make the changes and corrections and reshape it. With arthroscopic surgery, hip dislocation is not required. Osteotomy is done for pincer-type impingement.
Whenever possible, the surgeon tries to save the hip. When there is extensive damage to the cartilage, hip resurfacing or total joint replacement may be needed. There are many factors to consider when making the decision whether or not to do a hip replacement. These factors include the patient's age, findings on imaging studies, type and severity of deformity, as well as the presence of arthritic changes.
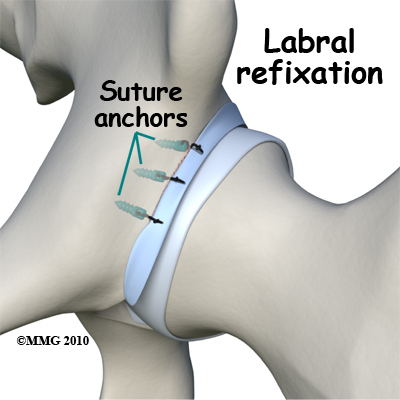
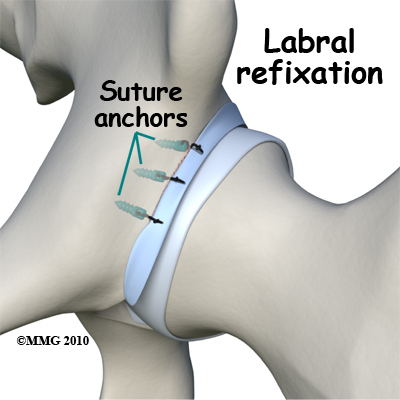
If there is a labral tear, surgery is usually done arthroscopically, whenever possible, to repair the damage. The surgeon trims the acetabular rim and then reattaches the torn labrum. This procedure is called labral refixation.
Each layer of tissue is sewn back together and reattached as closely as possible to its original position (called the footprint) along the acetabular rim. When repair is not possible, then debridement (shaving or removing) the torn tissue or pieces of tissue may be necessary.
Correction of the problem can result in improved function and pain relief. The hope is that early treatment can prevent arthritic changes but long-term studies have not been done to prove this idea.
After surgery, patients will be restricted to a partial weight-bearing status. The exact weight bearing recommendations will depend on the amount of bone removed and whether or not the labrum was torn and repaired.
Post-surgical Rehabilitation
What should I expect after surgery?
Rehabilitation at Beamsville Physiotherapy following surgery for FAI should begin as soon as your surgeon allows it. Each surgeon will set his own specific restrictions based on what was done during the surgical procedure, their personal experience, and whether your tissues are healing as expected. Generally speaking, the more complex the surgery the more involved and prolonged your rehabilitation program will be. In any case, activity restriction is important for the first few weeks after surgery in order to avoid fatiguing or overloading the hip muscles.
If you are still using crutches by the time we first see you at Beamsville Physiotherapy, your physiotherapist will ensure you are using the crutches safely, properly, and confidently and that you are abiding by your weight bearing restrictions. We will also ensure that you can safely use your crutches on stairs. If you are no longer using crutches, or once you no longer need them, your physiotherapist will focus on normal gait re-education so you are putting only the necessary forces through the surgical side with each step, and are not compensating in any way. Until you are able to walk without a significant limp, we recommend that you continue to use your crutches, or at least one crutch or a cane/walking stick. Improper gait can lead to a host of other pains in the knee, hip and back so it is prudent to use a walking aid until near normal walking can be achieved. Your physiotherapist at Beamsville Physiotherapy will advise you, along with recommendations from your surgeon, regarding the appropriate time for you to be walking without any walking aid at all.
During your first few appointments at Beamsville Physiotherapy your physiotherapist will focus on relieving any pain and inflammation you may still have from the surgical procedure itself. We may use modalities such as ice, heat, ultrasound, or electrical current to assist with decreasing any pain or swelling you have around the surgical site or anywhere down the limb. In addition, your physiotherapist may massage your hip, leg or ankle to improve circulation and help decrease your pain.
The next part of our treatment will focus on regaining normal range of motion in your hip. Your physiotherapist at Beamsville Physiotherapy will prescribe a series of stretching and strengthening exercises that you will practice in the clinic and also learn to do as part of a home exercise program. Range of motion in the hip generally comes back very quickly after surgery, but it still depends on what your surgeon has done inside your joint as well as the state of your joint prior to surgery. Rehabilitation will focus not only on regaining range of motion that may have been restricted due to the surgical process, but will particularly focus on improving flexibility and correcting imbalances that may have contributed to the impingement in the first place now that the anatomical issues have been corrected by the surgical procedure. Stretches for the front and back of your hip, particularly the hip flexors and the hip external rotators and abductors (deep gluteals) will be prescribed. An exercise bike at this stage is very useful to assist in gaining back the hip flexion and extension range of motion as long as the bike seat is kept high enough to avoid pinching of the hip during the flexion portion of the pedal cycle. Even if you are unable to fully rotate the pedals of the bike this activity it is still encouraged; performing the back and forth motion forces fluid through the joint and greatly assists the healing process.
If necessary your physiotherapist will mobilize your hip joint. This hands-on technique encourages the hip to move gradually into its normal range of motion. Mobilization of the hip may be combined with assisted stretching of any tight muscles around the surgical site. Particular attention will be taken such that the healing structures of the hip are not impinged at all during mobilizations of the area.
At Beamsville Physiotherapy we also highly recommend maintaining the rest of your body’s fitness with regular exercise while your hip is healing. This can begin very early post-surgically. You can use an upper body bike if you are non-weight bearing or may even be allowed to do aerobic exercises in a pool as long as it doesn’t compromise the hip. A stationary bike is often the best cardiovascular activity once the surgical structures have healed enough and you can put some weight through your foot. Weights for the upper extremities and other leg are also strongly encouraged. Your physiotherapist at Beamsville Physiotherapy can provide a program for you to maintain your general fitness while you recover from your surgery.
As soon as possible your therapist will prescribe strengthening exercises specifically for your surgical hip. These exercises will focus on restoring any muscle imbalances that have either been contributing to the impingement or that have developed due to the impingement. The deep gluteal muscles, in particular, will require specific attention as they are the major supporters of your hip joint, and also play a major role in controlling the position of your lower limb in standing. Exercises for your core area are also important and will be prescribed. Strengthening exercises that work the muscles while in standing most effectively assist with daily activities such as walking and stair climbing, however other very effective exercises for your gluteals in a lying position can be prescribed for the period while you are partial weight bearing. Your therapist may use an electrical muscle stimulator to assist your muscles in contracting as you do your exercises; this will help you to more rapidly gain your strength back. Exercises may also include the use of exercise bands or weights to provide added resistance for your hip and lower extremity. If you have access to a pool, your physiotherapist may suggest you go into the pool to do your exercises. The buoyancy of the water along with the warmth and hydrostatic properties can assist greatly in providing comfort to the hip joint and often allows your exercises to be done more easily with less discomfort. As soon as you are able, however, it is important to start land-based exercises as these more closely simulate your normal everyday activities.
As a result of any injury, the receptors in your joints and ligaments that assist with balance and proprioception (the ability to know where your body is without looking at it) decline in function. A period of immobility and reduced weight bearing will add to this decline. If your balance and proprioception has declined, your hip joint and your limb as a whole will not be as efficient in its functioning and this may contribute to injury in the future. As a final component of our treatment your physiotherapist at Beamsville Physiotherapy will prescribe exercises for you to regain balance and proprioception. These exercises might include activities such as standing on one foot or balancing on an unstable surface such as a wobbly board or a soft plastic disc. Advanced exercises will include agility type drills such as light hopping or moving side to side.
As your range of motion, strength, and proprioception improve, your physiotherapist will advance your exercises to ensure your rehabilitation is progressing as quickly as your body allows. As soon as it is safe to do so, your therapist will add more aggressive exercises such as jumping, hopping, and running, or exercises that mimic the sports or recreational activities that you enjoy participating in. During all of your exercises you physiotherapist will pay particular attention to your technique to ensure that you are not using any compensatory patterns or are developing bad habits in regard to how you use your hip and lower extremity. Enduring pain in your hip for years, months, or sometimes even just weeks usually causes you to use your hip and lower extremity in a pattern that avoids or limits your pain, but that is not efficient for a normal hip. If you do not pay close attention to how you use your joint and limb post-surgically these patterns often continue to occur once the source of your pain has been eliminated by surgery. Further hip impingement can occur. Your physiotherapist at Beamsville Physiotherapy will be crucial to providing you with feedback regarding correcting these patterns and developing new, efficient patterns during your daily activities.
Approximately five to six months after surgery your physiotherapist will guide you back to full activities including your sporting activities. Many patients report continued improvements in their symptoms even up to the end of the first year after surgery.
Generally the rehabilitation after surgery for FAI responds very well to the physiotherapy we provide at Beamsville Physiotherapy. If for some reason, however, your pain continues longer than it should or therapy is not progressing as your physiotherapist would expect, we will ask you to follow-up with your surgeon to confirm that the hip is tolerating the rehabilitation well and to ensure that there are no complications that may be impeding your recovery.
Portions of this document copyright MMG, LLC
Beamsville Physiotherapy provides services for physiotherapy in Beamsville.
 Femoroacetabular impingement (FAI) occurs in the hip joint. Impingement refers to some portion of the soft tissue around the hip socket getting pinched or compressed. Femoroacetabular tells us the impingement is occurring where the femur (thigh bone) meets the acetabulum (hip socket). There are two different types of impingement. They differ slightly depending on what gets pinched and where the impingement occurs.
Femoroacetabular impingement (FAI) occurs in the hip joint. Impingement refers to some portion of the soft tissue around the hip socket getting pinched or compressed. Femoroacetabular tells us the impingement is occurring where the femur (thigh bone) meets the acetabulum (hip socket). There are two different types of impingement. They differ slightly depending on what gets pinched and where the impingement occurs.








 Femoroacetabular refers to the place in the hip where the round head of the femur (thigh bone) comes in contact with the acetabulum or hip socket. Two types of impingement are known to cause pinching of the soft tissues in this area: The first is called cam-type impingement. This occurs when the round head of the femur isn't as round as it should be. It's more of a pistol grip shape.
Femoroacetabular refers to the place in the hip where the round head of the femur (thigh bone) comes in contact with the acetabulum or hip socket. Two types of impingement are known to cause pinching of the soft tissues in this area: The first is called cam-type impingement. This occurs when the round head of the femur isn't as round as it should be. It's more of a pistol grip shape.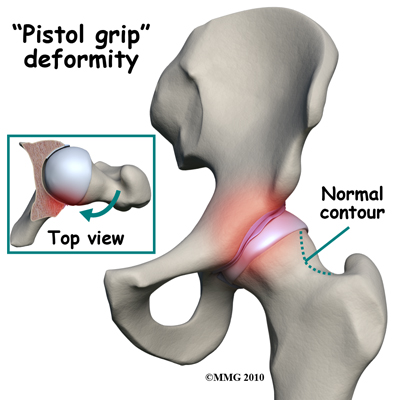
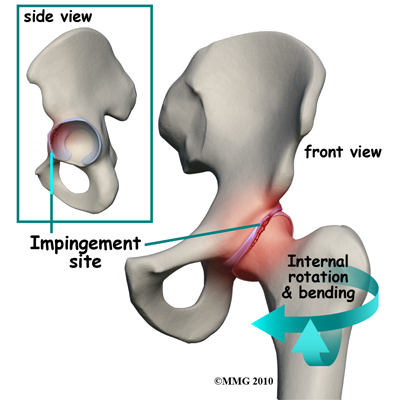 Normally, the femoral head moves smoothly inside the hip socket. The socket is just the right size to hold the head in place. If the acetabulum is too shallow or too small, the hip can dislocate. In the case of FAI, the socket may be too deep.
The rim of the cartilage hangs too far over the head. When the femur flexes (bends) and internally rotates, the cartilage gets pinched. Over time, this pinching or impingement of the labrum can cause fraying and tearing of the edges and/or osteoarthritic changes at the impingement site.
At the same time, with changes in the shape and structure of the hip, there are changes in normal hip movement. There may be too much hip adduction and internal rotation. Hip adduction refers to movement of the leg toward the body. Muscle weakness of the hip abductor muscles, hip extensors, and hip external rotators add to the problem. Hip abduction is moving the leg away from the body.
With the combined effects of anatomic changes in the hip and the resultant muscle imbalances, repetitive motions can create mini-traumas to the hip joint. The result can be an additional problem: partial or complete labral tears. A complete rupture is referred to as an avulsion which indicates that the labrum is separated from the acetabular cartilage where it normally attaches.
Normally, the femoral head moves smoothly inside the hip socket. The socket is just the right size to hold the head in place. If the acetabulum is too shallow or too small, the hip can dislocate. In the case of FAI, the socket may be too deep.
The rim of the cartilage hangs too far over the head. When the femur flexes (bends) and internally rotates, the cartilage gets pinched. Over time, this pinching or impingement of the labrum can cause fraying and tearing of the edges and/or osteoarthritic changes at the impingement site.
At the same time, with changes in the shape and structure of the hip, there are changes in normal hip movement. There may be too much hip adduction and internal rotation. Hip adduction refers to movement of the leg toward the body. Muscle weakness of the hip abductor muscles, hip extensors, and hip external rotators add to the problem. Hip abduction is moving the leg away from the body.
With the combined effects of anatomic changes in the hip and the resultant muscle imbalances, repetitive motions can create mini-traumas to the hip joint. The result can be an additional problem: partial or complete labral tears. A complete rupture is referred to as an avulsion which indicates that the labrum is separated from the acetabular cartilage where it normally attaches.
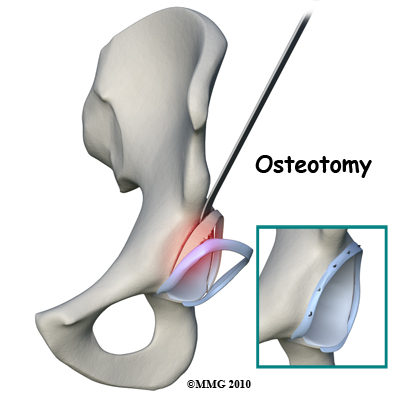 With the fully open surgical procedure, the head of the femur is dislocated from the socket to make the changes and corrections and reshape it. With arthroscopic surgery, hip dislocation is not required. Osteotomy is done for pincer-type impingement.
Whenever possible, the surgeon tries to save the hip. When there is extensive damage to the cartilage, hip resurfacing or total joint replacement may be needed. There are many factors to consider when making the decision whether or not to do a hip replacement. These factors include the patient's age, findings on imaging studies, type and severity of deformity, as well as the presence of arthritic changes.
With the fully open surgical procedure, the head of the femur is dislocated from the socket to make the changes and corrections and reshape it. With arthroscopic surgery, hip dislocation is not required. Osteotomy is done for pincer-type impingement.
Whenever possible, the surgeon tries to save the hip. When there is extensive damage to the cartilage, hip resurfacing or total joint replacement may be needed. There are many factors to consider when making the decision whether or not to do a hip replacement. These factors include the patient's age, findings on imaging studies, type and severity of deformity, as well as the presence of arthritic changes.